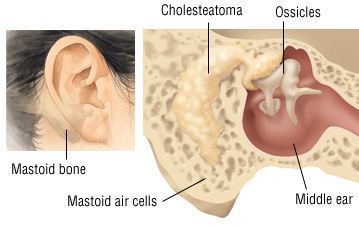
Chronic suppurative otitis media (CSOM) is a chronic inflammation of the middle ear and mastoid cavity. Clinical features are recurrent ear discharge through a tympanic perforation, with hearing loss of varying severity.
The tympanic membrane is perforated in CSOM. If this is a tubotympanic perforation, it is usually ‘safe’, whilst atticoantral perforation is often ‘unsafe’. Safe or unsafe depends on the presence of cholesteatoma:
- Safe CSOM is CSOM without cholesteatoma. It can be subdivided into active or inactive depending on whether or not infection is present.
- Unsafe CSOM involves cholesteatoma. Cholesteatoma is a non-malignant but destructive lesion of the skull base.
Risk factors
- Multiple episodes of acute otitis media (AOM).
- Living in crowded conditions.
- Being a member of a large family.
- Attending daycare.
- Socioeconomic status.
- Craniofacial anomalies increase risk: cleft lip or palate, Down’s syndrome, cri du chat syndrome, choanal atresia, and microcephaly all increase the risk of CSOM.
Symptoms
- CSOM presents with a chronically draining ear (>2 weeks), with a possible history of recurrent AOM, traumatic perforation, or insertion of grommets.
- The otorrhea should occur without otalgia or fever.
- Fever, vertigo and otalgia should prompt urgent referral to exclude intratemporal or intracranial complications.
- Hearing loss is common in the affected ear. Mixed hearing loss (conductive and sensorineural) suggests extensive disease.
Signs
- The external auditory canal may possibly be oedematous but is not usually tender.
- The discharge varies from fetid, purulent and cheese-like to clear and serous.
- Granulation tissue is often seen in the medial canal or middle ear space.
- The middle ear mucosa seen through the perforation may be oedematous or even polypoid, pale, or erythematous.
Investigations
- An audiogram will normally show conductive hearing loss. Mixed hearing loss may suggest more extensive disease and possible complications.
- X-ray Mastoids lateral oblique view.
- A fine-cut CT scan can reveal bone erosion from cholesteatoma, ossicular erosion, involvement of petrous apex and subperiosteal abscess.
- MRI is better if intratemporal or intracranial complications are suspected.
Management
Conservative treatment of CSOM consists of 3 components:
- An appropriate antibiotic.
- Regular intensive aural toilet to remove debris.
- Control of granulation tissue.
Surgical
- In safe inactive CSOM, once infection has been controlled, a tympanoplasty is usual to prevent recurrent infection.
- Surgery is required in unsafe CSOM, as cholesteatoma can cause serious and possibly fatal complications. Classical radical mastoidectomy, modified radical mastoidectomy or the ‘combined approach tympanoplasty’ may be used depending on the extent of cholesteatoma and, more importantly, the experience of the surgeon. Whatever the procedure chosen, the aim of surgery is to remove all disease and to give the patient a dry and functioning ear.
- Facial paralysis can occur with or without cholesteatoma. Surgical exploration with mastoidectomy should be undertaken promptly.
- Where conductive hearing loss has resulted from CSOM (due to perforation of the tympanic membrane and/or disruption in the ossicular chain), surgical removal of the infection and cholesteatoma, followed by ossicular chain reconstruction, will reduce hearing loss.
Complications
Complications of CSOM are rare but potentially life-threatening.
Intratemporal complications include:
- Petrositis
- Facial paralysis
- Labyrinthitis
Intracranial complications include:
- Lateral sinus thrombophlebitis
- Meningitis
- Intracranial abscess
Sequelae include:
- Hearing loss
- Tympanosclerosis
Prognosis
- There is a good chance of control of infection.
- The recovery of hearing loss varies, depending on the cause. Conductive hearing loss often can be partially corrected with surgery.