Perforations do not always heal with medical management alone. Thus, in some cases, microsurgery may be necessary to close the perforation. This surgery is called tympanoplasty.
Long-standing perforations can be more severe due to infection and erosion of the bones of hearing, which disrupt the bony chain of the middle ear. An audiogram (hearing test) is taken to determine the degree of hearing loss. If the hearing loss is mild and hearing improves upon patching of the hole, then almost certainly the bones of hearing (ossicular chain) are intact. Thus, reconstruction of the eardrum will be a curative procedure. However, when there is a larger hearing loss, there is very likely to be damage to the bones of hearing. There is no way to determine the status of the bones of hearing preoperatively in this situation.
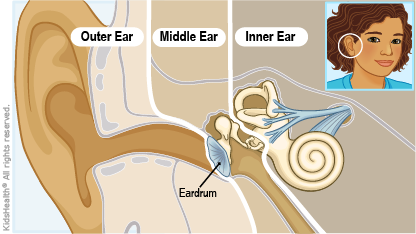
Very active infection which does not dry up with standard techniques may indicate that there is an infection in the mastoid bone. The mastoid bone is the hard bone that you feel if you press behind your ear. Within this bone, there is an air-filled space called the mastoid cavity. This air-filled space connects with the middle ear which is also air filled. Infections of the middle ear can spread into the mastoid cavity causing a more serious infection called mastoiditis. A CT scan may be necessary to evaluate this possibility further.
Surgery to reconstruct the tympanic membrane (eardrum) can be performed under general anaesthesia. The operating microscope helps to enlarge the view of the ear structures, giving a more detailed image to the ear surgeon. It is performed by an incision behind the ear. This elevates the entire outer ear forward, gaining access to the perforation. Once the hole is exposed fully, the perforated remnant is rotated forward, and the bones of hearing are inspected. There may be scar tissue and bands surrounding the bones of hearing. These can be removed with micro hooks.
Having identified the bones of hearing, the ossicular chain is pressed to determine if the chain is mobile and functioning. If the chain is mobile, then the remaining surgery concentrates on repairing the drum defect.
A tissue is taken either from the back of the ear or from the small cartilaginous lobe of skin in front the ear called the tragus. The tissues are thinned and dried. An absorbable gelatin sponge is placed under the drum to allow for support of the graft. The graft is then inserted underneath the remaining drum remnant and the drum remnant is folded back onto the perforation to provide closure. Absorbable packing is done to fill the ear canal above the graft. Sterile packing is done to cover the rest of the ear canal.
The ear is then stitched together. A sterile dressing is done to cover the ear. After about ten days, the packing and stitches are removed and a good evaluation can then be obtained as to whether the graft was successful. Water is kept away from the ear and blowing of the nose is discouraged. If there are allergies or cold, further antibiotics and decongestant should be given.
In over 90% of cases, the tympanoplasty procedure is successful and a hearing test is performed at four to six weeks after the operation. If the bones of hearing are eroded, then ossicular reconstruction (reconstruction of the bones of hearing) may be necessary at the time of tympanoplasty. In some cases, this can be determined before the surgery. In other cases, it only becomes obvious at the time that the ear is completely opened and examined under the microscope.
Selection and Results
Tympanoplasty surgery is not always recommended. Chronic sinus or nasal problems such as severe allergies make the operation more difficult. They must be cleared up or controlled prior to tympanoplasty surgery.
The ear and nose are connected by the eustachian tube. If there is an active infection in the sinuses or nose, infected materials may block the eustachian tube or even back up into the tube itself. Severe allergies may cause swelling of the tube which is normally lined with mucous membranes. Unless allergies are controlled, the swelling will block the eustachian tube and surgical attempts to repair the eardrum will fail.
If most of the eardrum is absent and the ossicles are destroyed by prior infection or disease, reconstruction will have to be staged into several operations. The first-stage operation reconstructs the eardrum. The second-stage operation, performed six months to one year later, addresses the reconstruction of the bones of hearing.
Mastoid infection, if present, may require that tympanoplasty surgery include mastoidectomy. The mastoid cavity may contain a reservoir of infection. If this material is not cleaned out, the new eardrum will break down after initial success. Thus, it is advisable to obtain a CT scan to visualize the mastoid cavity, if there is a history of prolonged and resistant infection. If the mastoid cavity appears diseased, the tympanoplasty with combined mastoidectomy is often recommended. This operation, termed tympanomastoidectomy, not only involves repairing the eardrum but during the same operation, the mastoid bone is opened with a drill and all diseased tissue is removed. This procedure may lengthen the operation by 45 minutes or more, but it will improve the chance of a successful result.